Epidemiology
- Potentially malignant disorder of the lips caused by long-term exposure to solar radiation.
- Frequency is higher in geographical areas with high ultraviolet (UV) radiation, in open-air workers and in those with fairer skin types.
- More common among individuals >50 years with long periods of exposure to solar light but can occur at any age
- Other factors that have been associated include low educational level, a precarious socioeconomic status, genetic predisposition and unhealthy lifestyles such as smoking and poor diet
- Rates of malignant AC transformation to squamous cell carcinoma have not been definitively established. A number of studies have estimated the rate at between 3.07% – 17%.
- Up to 95% of cases of SCC of the lips are preceded by AC
Clinical Presentation
- Most commonly affects the lower lip and presents with a broad range of clinical characteristics.
- Initially characterized by redness, flaking, induration, erosion and/or cracks or ulcers on the vermilion. Repeated exposure to UV radiation produces chronic tissue changes including hyperkeratosis, loss of elasticity and effacement of the cutaneous-mucous labial border (Figure 1). These manifestations can be localized or diffuse.
- First clinical signs of AC can be subtle, and patients may attribute these changes to normal aging. As a result, the time to initial presentation is often delayed until more advanced changes or SCC is already present.

Differential Diagnosis
Herpes simplex infection, lichen planus, oral lichenoid lesions, erythema multiforme, pemphigus vulgaris, leukoplakia, SCC, basal cell carcinoma, malignant melanoma and other forms of cheilitis such as exfoliative cheilitis and contact cheilitis.
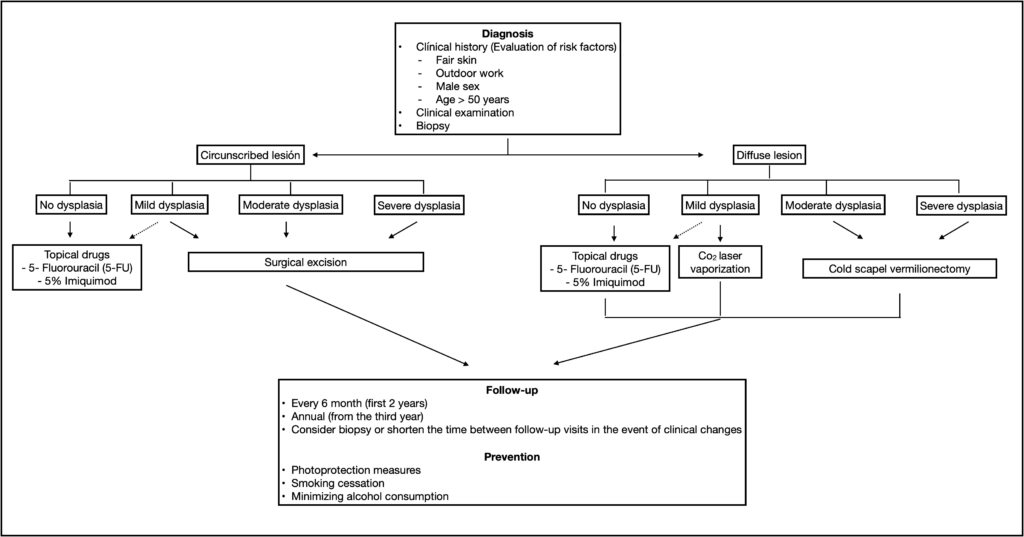
Diagnosis
- The diagnosis of AC is based on the demographic history, clinical findings and histopathology
- Effacement of the vermilion border is a relevant clinical characteristic but can be difficult to identify due to the loss of support of the labial structures in older patients
- On palpation, AC is often perceived as fine sandpaper when sliding a gloved finger over the surface of the lip. Palpation is also important to differentiate AC from SCC of the lips. The neck should also be examined for the presence of lymphadenopathy (unilateral v. bilateral, mobile vs. fixed).
- Diagnosis is usually clinical, but a confirmatory biopsy should be undertaken, especially on lesions that demonstrate substantial changes, such as induration, ulceration, and suspicious of an SCC
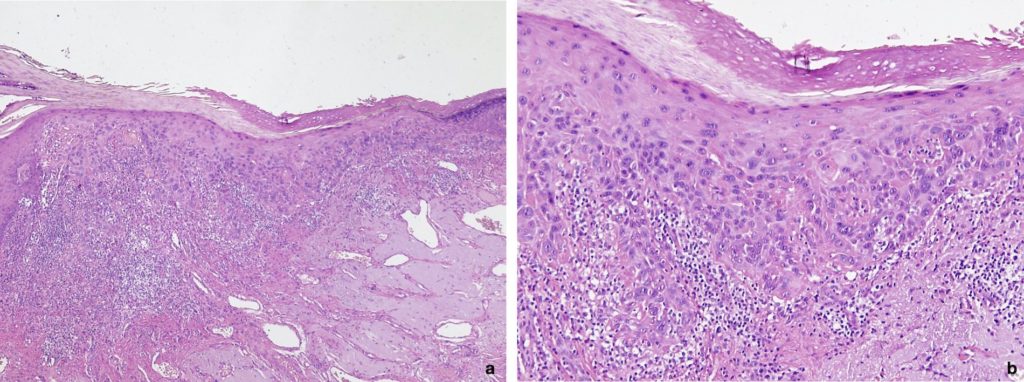
- Histologically, AC causes changes at an epithelial level and in the underlying connective tissue. The epithelium in AC can present hyperkeratosis, hyperparakeratosis, atrophy, acanthosis or loss of polarity of the basal keratinocytes. Varying degrees of dysplasia is frequent.
Management
Prevention
Adequate photoprotection is the important preventative measure for AC. This includes:
- Limiting exposure to the sun between 10 am and 2 pm (or between 11 am and 3 pm in summer)
- Wearing a protective wide-brimmed hat
- Using water-resistant lip balm with broad-spectrum UVA and UVB protection (SPF30+), applied generously and reapplied at least every 2 hours.
Treatmen
- Aim of treatment is to reduce the risk of malignant transformation while maintaining functionality and aesthetics.
- Various surgical and non-surgical therapeutic options have been employed aimed at eliminating dysplastic epithelium.
- Type of therapeutic modality should depend on the individual case and based on the clinical (size, location) and pathology findings (degree of epithelial dysplasia), taking into account side effects, potential aesthetic sequelae and evidence base
Non-Surgical Therapy
- The most common non-surgical therapies include topical applications of fluorouracil (5-FU), 5% imiquimod, 3% diclofenac with 2.5% hyaluronic acid, and 0.015% ingenol mebutate
- Photodynamic therapy, which consists of combining a light source (400-700 nm) and a photosensitizer (5–20% 5-aminolevulinic acid or methyl aminolevulinate), produces free oxygen radicals that destabilize the membranes and cell organelles, inducing cell death
- Non-surgical therapies are less invasive and have fewer side effects than surgical modalities. However, they are less effective in terms of clinical and histological control of the lesion and associated with higher relapse rates.
- Topical therapies can improve results when used in conjunction with surgical therapeutic options
Surgical Therapy
- Vermilionectomy by excision – should be reserved for diffuse AC with moderate to severe dysplasia
- Laser ablation – should be employed for diffuse or multisite lesions with mild dysplasia
- Cryotherapy
- Electrocauterization
Localized lesions suspicious for malignancy should undergo excision or vaporization if moderate to severe dysplasia is detected, or complete surgical excision if an SCC is diagnosed.
Follow-up
- AC treatment should be supplemented with sun protection creams and periodic clinical reviews
- Patients should undergo a post-therapy follow-up regimen, with visits at least every 6 months during the first 2 years and subsequently annually
- If changes are detected during follow-up, re-biopsy should be performed, and follow-up intervals shortened.
References and Further Reading
Cataldo E, Doku HC. Solar cheilitis. J Dermatol Surg Oncol. 1981 Dec;7(12):989-95.
Warnakulasuriya S, Kujan O, Aguirre-Urizar JM, Bagan JV, González-Moles MÁ, Kerr AR, Lodi G, Mello FW, Monteiro L, Ogden GR, Sloan P, Johnson NW. Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer. Oral Dis. 2020 (In press)
Junqueira JL, Bönecker M, Furuse C, Morais Pde C, Flório FM, Cury PR, Araújo VC. Actinic cheilitis among agricultural workers in Campinas, Brazil. Community Dent Health. 2011;28(1):60-3.
Ferreira AM, de Souza Lucena EE, de Oliveira TC, da Silveira É, de Oliveira PT, de Lima KC. Prevalence and factors associated with oral potentially malignant disorders in Brazil’s rural workers. Oral Dis. 2016;22(6):536-42.
Tortorici S, Corrao S, Natoli G, Difalco P. Prevalence and distribution of oral mucosal non-malignant lesions in the western Sicilian population. Minerva Stomatol. 2016; 65(4):191-206.
Ntomouchtsis A, Karakinaris G, Poulolpoulos A, Kechagias N, Kittikidou K, Tsompanidou C, Vahtsevanos K, Antoniades K. Benign lip lesions. A 10-year retrospective study. Oral Maxillofac Surg. 2010;14(2):115-8.
Rodríguez-Blanco I, Flórez Á, Paredes-Suárez C, Rodríguez-Lojo R, González-Vilas D, Ramírez-Santos A, Paradela S, Suárez Conde I, Pereiro-Ferreirós M. Actinic Cheilitis Prevalence and Risk Factors: A Cross-sectional, Multicentre Study in a Population Aged 45 Years and Over in North-west Spain. Acta DermVenereol. 2018;98(10):970-974.
Kaugars GE, Pillion T, Svirsky JA, Page DG, Burns JC, Abbey LM. Actinic cheilitis: a review of 152 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(2):181-6.
de Souza Lucena EE, Costa DC, da Silveira EJ, Lima KC. Prevalence and factors associated to actinic cheilitis in beach workers. Oral Dis. 2012;18(6):575-9.
Vieira R, Minicucci EM, Marques ME, Marques SA. Actinic cheilitis and squamous cell carcinoma of the lip: clinical, histopathological and immunogenetic aspects. An Bras Dermatol. 2012;87:105‐114.
Jadotte YT, Schwartz RA. Solar cheilosis: an ominous precursor: part I. Diagnostic insights. J Am Acad Dermatol. 2012;66(2):173-84.
Markopoulos A, Albanidou-Farmaki E, Kayavis I. Actinic cheilitis: clinical and pathologic characteristics in 65 cases. Oral Dis. 2004;10(4):212-6.
Dancyger A, Heard V, Huang B, Suley C, Tang D, Ariyawardana A. Malignant transformation of actinic cheilitis: A systematic review of observational studies. J InvestigClinDent. 2018;9(4):e12343.
Gomes JO, de Vasconcelos Carvalho M, Fonseca FP, Gondak RO, Lopes MA, Vargas PA. CD1a+ and CD83+ Langerhans cells are reduced in lower lip squamous cell carcinoma. J Oral Pathol Med. 2016;45(6):433-9.
Lai M, Pampena R, Cornacchia L, Pellacani G, Peris K, Longo C. Treatments of actinic cheilitis: A systematic review of the literature. J Am Acad Dermatol. 2020 Sep;83(3):876-887.
Savage NW, McKay C, Faulkner C. Actinic cheilitis in dental practice. Aust Dent J. 2010;55 Suppl 1:78-84.
Van der Waal. Queilitis Actínica. In: Bascones A, Seoane JM, Aguado A, Suárez-Quintanilla JM. Cáncer y precáncer oral: Bases clínico-quirúrgicas y moleculares. Ediciones Avances Médico-Dentales S.L., Madrid, 2003.
Muse ME, Crane JS. Actinic Cheilitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020.
Jadotte YT, Schwartz RA. Solar cheilosis: an ominous precursor part II. Therapeutic perspectives. J Am Acad Dermatol. 2012;66(2):187-98.
Greenberg SA, Schlosser BJ, Mirowski GW. Diseases of the lips. Clin Dermatol. 2017 Sep-Oct;35(5):e1-e14.
Ulrich M, González S, Lange-Asschenfeldt B, Roewert-Huber J, Sterry W, Stockfleth E, Astner S. Non-invasive diagnosis and monitoring of actinic cheilitis with reflectance confocal microscopy. J Eur Acad Dermatol Venereol. 2011;25(3):276-84.
Kahn MA, Hall JM. The ADA practical guide to soft tissue oral disease. 2nd edition. Wiley, 2018.
Warnakulasuriya S (2000). Lack of molecular markers topredict malignant potential of oral precancer. J Pathol 190:407–409.
Mello FW, Miguel AFP, Dutra KL, Porporatti AL, Warnakulasuriya S, Guerra ENS, Rivero ERC. Prevalence of oral potentially malignant disorders: A systematic review and meta-analysis. J Oral Pathol Med. 2018;47(7):633-640.
Onofre MA, Sposto MR, Navarro CM, Motta ME, Turatti E, Almeida RT. Potentially malignant epithelial oral lesions: discrepancies between clinical and histological diagnosis. Oral Dis 1997; 3: 148–152.
Menta Simonsen Nico M, Rivitti EA, Lourenço SV. Actinic cheilitis: histologic study of the entire vermilion and comparison with previous biopsy. J Cutan Pathol. 2007;34(4):309-14.
Rodriguez-Blanco I, Florez Á, Paredes-Suárez C, Rodríguez-Lojo R, González-Vilas D, Ramírez-Santos A, Paradela S, Suárez Conde I, Pereiro-Ferreirós M. Use of lip photoprotection in patients suffering from actinic cheilitis. Eur J Dermatol. 2019;29(4):383-386.
Salgueiro AP, de Jesus LH, de Souza IF, Rados PV, Visioli F. Treatment of actinic cheilitis: a systematic review. Clin Oral Investig. 2019;23(5):2041-2053.
Varela-Centelles P, Seoane-Romero J, García-Pola MJ, Leira-Feijoo Y, Seoane-Romero JM. Therapeutic approaches for actinic cheilitis: therapeutic efficacy and malignant transformation after treatment. Int J Oral Maxillofac Surg. 2020;49(10):1343-1350.
Calcaianu N, Popescu SA, Diveica D, Lascar I. Surgical attitude in premalignant lesions and malignant tumors of the lower lip. J Med Life. 2015;8(1):109-11.
Carvalho MV, de Moraes SLD, Lemos CAA, Santiago Júnior JF, Vasconcelos BCDE, Pellizzer EP. Surgical versus non-surgical treatment of actinic cheilitis: A systematic review and meta-analysis. Oral Dis. 2019;25(4):972-981.
Trager MH, Farmer K, Ulrich C, Basset-Seguin N, Herms F, Geskin LJ, Bouaziz JD, Lebbé C, de Masson A, Bagot M, Dobos G. Actinic cheilitis: a systematic review of treatment options. J Eur Acad Dermatol Venereol. 2020 (In press)







